Rotation 2
Ambulatory Medicine: Centers Urgent Care
Focused H&P 1:
Name: M.J
Sex: Male
DOB: 1/5/68
Date: 16Feb20 at 1130
Ethnicity: Caucasian
Marital status: Married
Religion: None
Information: Self-religion
Source of Referral: Self
52 y/o deaf male with PMH of splenectomy presents to urgent care clinic c/o sore throat and cough x 3 weeks. Pt had to communicate via pen/paper and states sxs have gotten worse. Cough is productive of yellow sputum and it keeps him awake at night. The sore throat has gotten worse and is painful 7/10 pain non-radiating. Admits to feverish chills, loss of appetite, abdominal pain. Last oral intake was this morning, cereal. LBM yesterday, “normal” no blood noted. Denies self tx, N/V/D, HA, blurry vision, SOB, chest pain, wheezing, hemoptysis, palpitations, trauma or LOC.
PMH: deaf since birth both ears.
- Splenectomy secondary to “benign” tumor.
- Born without left pectoralis major muscle.
Denies recent hospitalizations
FH: None pertinent to chief complaint
ALL: NKDA
Meds: None.
Social hx: former smoker 1ppd x 10 years quit in 2010. Denies ETOH or illicit drugs.
ROS: See HPI.
Physical exam:
WNWD male NAD A&OxIII.
Vitals: 146/88 Pulse 98 Resp 22. Temp 101.0, SpO2 94% RA. Height: 69” weight: 163
Head: normocephalic atraumatic
Eyes: Symmetrical, Iris blue. No injection/jaundice over sclera. EMOI without nystagmus. PERRLA.
Ears: symmetrical. No TTP over tragus, helix, lobe. AU-EAC unobstructed. TMs pearly gray with all landmarks visible. No injection or discharge noted. Whisper test deferred
Nose: Patent airway. No inflamed turbinates. No rhinorrhea.
Mouth/throat: Tongue, uvula midline. Teeth intact. Noted PND on posterior pharynx. No erythema or cobble-stoning over tonsils, tonsils at grade +2.
Lymph: No palpable/tender lymphadenopathy.
Lungs: Inspection of chest revealed missing pectoralis major muscle absent. Nipple intact. No discharge from nipple. Crackles/wheezing noted over posterior left lower lobe on inspiration/expiration. Did not clear to cough. Lungs clear to auscultation in all other fields. No dullness to percussion. Thoracic expansion adequate.
Heart: RRR without gallops, skips or murmurs.
Abdomen: Noted 10cm scar well healed over umbilicus (2/2 splenectomy). Noted TTP over LUQ with light/deep. Bowel sounds heard throughout. Neg murphy’s sign, obturator or psoas sign.
Skin: Warm/moist. No evidence of jaundice or cyanosis.
DDx @ this time:
- Pneumonia
- Bronchitis
- Upper respiratory infection
- Gastritis
- Cholecystitis
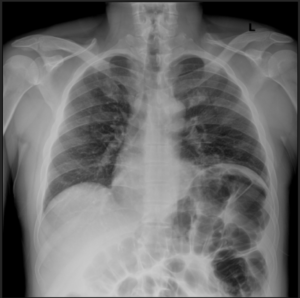
Results from Chest X-ray:
- Frontal and lateral views of the chest reveal basilar atelectatic changes on the left side in association with an elevated left hemidiaphragm. Lung volumes are generally, by submaximal inspiration. There is no evidence of pneumonia demonstrated on either side.
- Heart size is normal.
- No pleural fluid collections are seen.
- Incidental note is made of somewhat diffuse gaseous distention of the colon suggestive of possibility of a colonic ileus.
Impression: Atelectatic, diaphragmatic and colonic changes as described above. No evidence of pneumonia.
New DDx:
- Ileus
- SBO
- LBO
- Volvulus
- Peritonitis
Assessment/Plan:
52 y/o male with PMH deafness and splenectomy c/o cough, sore throat, & epigastric pain presenting with suspected colonic ileus based on radiographic finding.
Advised pt NPO
Advised pt to report to local ER for further evaluation and treatment
Pt notified next of kin via text to arrange pick up to local emergency department.
911/ambulance service was offered and declined.
Focused H&P 2
Name: L.G
Sex: Male
DOB: 07/03/2012
Date: 17Feb20 at 1330
Ethnicity: Hispanic
Marital status: Single
Religion:
Information: Self-religion
Source of Referral: Self/mother
7 y/o male presents to urgent care c/o severe right ear pain since yesterday. Pt was seen at an urgent care in Florida and dx with right otitis media and Rx z-pac, Sudafed, and ibuprofen. Pt was flying home yesterday and heard/felt a loud pain and was in terrible pain. Pt has previous hx of recurrent/chronic otitis media. Mother noted clear and bloody discharge coming from right ear since yesterday. Pt states it sounds loud and feels that he cannot hear. Denies F/C, SOB, chest pain, vertigo, head trauma, or neck pain.
PMH: Myringotomy 2014 and again 2016.
Recurrent otitis media both ears.
FH: Both parents healthy
ALL: Peanutsà rash
Meds: Azithromycin pack
- Sudafed 30mg
- Ibuprofen liquid
Surgical: Myringotomy 2014 and 2016.
Physical exam:
WNWD female NAD A&OxIII.
Vitals: Pulse 129 Resp 18. Temp 96.9, SpO2 96% RA. Height: 49” weight: 53
Head: normocephalic atraumatic
Eyes: Symmetrical, Iris brown. No injection/jaundice over sclera. EMOI without nystagmus. PERRLA.
Ears: symmetrical. Mild TTP over right tragus. No mastoid tenderness. AD TM retracted with noted 3mm length laceration at the 9 o’clock position. Unable to visualize landmarks. Noted bloody discharge in the EAC. AS-EAC unobstructed, TM pearly gray with all landmarks visible. No injection or discharge noted.
Nose: Patent airway. No inflamed turbinates. No rhinorrhea.
Mouth/throat: Tongue, uvula midline. Teeth intact. Tonsils at grade +1.
Lymph: No palpable/tender lymphadenopathy.
Lungs: No adventitious lung sounds.
Heart: RRR without gallops, skips or murmurs.
Skin: Warm/moist. No evidence of jaundice or cyanosis.
DDx:
- Otitis Media
- Tympanic membrane perforation
- Otitis externa
- Mastoiditis
- Assessment/plan
7 y/o male with no PMH presenting to urgent care with otitis media and suspected tympanic membrane perforation. In structed pt to continue medications as prescribed and recommended pt to see peditrican and ENT specialist. Recommended initial consult with audiologist if needed.
Educated pt to keep ear canal dry and not to administer any medications into the ear. No swimming or flying for 30 days.
20Feb20 at 1800
Pt presents to urgent care again with pain in left ear. Pt was seen 3 days ago with RIGHT ear pain and now the pain is severe in his left. He was blowing his nose and felt a pop in his left ear. Pain has been somewhat controlled with ibuprofen and has no other symptoms. He denies fever/chills, SOB, chest pain, neck pain, vertigo.
WNWD female NAD A&OxIII.
Vitals: Pulse 118 Resp 18. Temp 99.9, SpO2 98% RA. Height: 49” weight: 53
Head: normocephalic atraumatic
Eyes: Symmetrical, Iris brown. No injection/jaundice over sclera. EMOI without nystagmus. PERRLA.
Ears: symmetrical. No mastoid tenderness. AD TM retracted with noted 6mm length laceration at the 2 o’clock position. Unable to visualize landmarks. Noted bloody discharge in the EAC. Right ear still shows obvious TM perforation. No discharge or blood noted.
Nose: Patent airway. No inflamed turbinates. No rhinorrhea.
Mouth/throat: Tongue, uvula midline. Teeth intact. Tonsils at grade +1.
Lymph: No palpable/tender lymphadenopathy.
Lungs: No adventitious lung sounds.
Heart: RRR without gallops, skips or murmurs.
Skin: Warm/moist. No evidence of jaundice or cyanosis.
Assessment/plan
7 y/o male with no PMH presenting to urgent care with otitis media and suspected tympanic membrane perforation. Pt was seen by pediatrician and Rx Augmentin and was told to discontinue the azithromycin. Pt was told to f/u with pediatrician as stated and it was recommended to see ENT specialist.
____________________________________________________________________
Article
What is Meniere’s disease A contemporary re-evaluation of endolymphatic hydrops
This article provides an overview of Meniere’s Disease and I chose it because I had a suspected patient who may have been diagnosed with this disease. Meniere’s Disease is also known as endolymphatic hydrops and affects the ear. This article lays out the definition of the disease, the known pathophysiology, clinical manifestations, diagnostic studies, treatment and prognosis. I had assumed Menier’s disease was a basic diagnosis made on the triad (vertigo, hearing loss and tinnitus), however that is not the case. Patients need constant evaluations by otolaryngologists and audiologists, and most cases the diagnosis takes 3-5 years. This article provided an in-depth list of treatment options including pharmacological and surgical options for patients with Meniere’s. It would be an article that I reference in the future to strengthen my knowledge on Meniere’s Disease.
____________________________________________________________________
Typhon:
____________________________________________________________________
Site Evaluator Reflection
My site evaluation went well. The site evaluator liked my cases that I brought and noted they were interesting. The first focused H&P listed above was one of the ones I presented. Some of the other focused H&Ps needed a longer list of differentials based on the clinical scenario given and it is something that I need to work on the future. Differentials is a difficult part of being a clinician. At times the symptoms blend together and diseased systems overlap. This makes it difficult to have a concise list that is appropriate to make the proper diagnosis.
____________________________________________________________________
Rotation Summary:
Ambulatory Medicine is a great experience and an important aspect of healthcare. The urgent care that I worked at provided quick care to patients in need and provided a great learning experience. The preceptor challenged me to provide adequate and compassionate healthcare with minimal tools and diagnostics. This was the first tool that I learned with at the urgent care, stick with your clinical knowledge. Having the ability to take a strong history and a thorough exam provides a great foundation to accurately diagnose patients. This led to another important aspect which was repetition. Every patient that presented with upper respiratory symptoms I evaluated the same way. This allows the practitioner to understand what is “normal” and what is not.
Another task that my preceptor instilled on me was to present patients without writing down notes. This was difficult in the beginning but it forced habits of how to ask questions. I kept on repeating questions to patients in the beginning because I was not used to this new idea. Secondly, there were certain questions I would repeat throughout my exam, one of which was, “do you have any allergies?” I would ask that question a number of times during an examination and it reiterate the need thoroughness and do-diligence. Another “trick” that I learned while not taking notes during an exam is that I pictured the template on the computer when assessing patients.
During this ambulatory medicine rotation I saw a wide range of medical conditions ranging from bronchitis and otitis media, to colonic ileus and fractured lateral malleolus. These wide variety of conditions kept you on your toes and it focused on an accurate list of differential diagnosis. For example, a patient presented with 5 days of unilateral facial numbness and pain. My differential was long and varied and including the following:
- sinusitis
- bells palsy
- trigeminal neuralgia
- optic neuritis
- Temporal arteritis
- Stroke
- TIA
I needed to rule out each of these based on my history taking and clinical skills. The diagnosis was sinusitis. Urgent care setting does not give you a lot of time to figure out a diagnosis and provide treatment at your pace. Patients need to know if they need further evaluation and treatment at the hospital. On a number of occasions patients would present to urgent care in their own vehicle but would leave in an ambulance.
I cannot fully describe what I have learned in detail because I have learned a large amount of little particulars that are difficult to put into words. I truly hope that other PA students in my class and other students in the healthcare field can benefit from an urgent care setting as much as I have.


