Rotation #1
General Surgery. WoodHull Hospital Brooklyn
H&P:
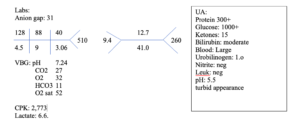
26 y/o African American male with unknown PMH presents to ER with AMS after at home c/o testicular pain, pt was found by mother, present in possible DKA, pt noted to be non-compliant with DM medication (insulin & metformin). Mother is speaking on behalf of patient due to mental status. Pt denies head trauma, or falling.
No surgical history
Unable to obtain family hx.
Denies TOB use. Denies ETOH use
ROS: unable to obtain ROS due to mental status change
WNWD obese male, appears appropriate age and is well groomed.
BP: 131/82 Pulse 145 Temp 99.0 Resp 40 SPO2 98 122kg 75” BMI 33.75
Head: Normocephalic,.
Eyes: Symmetrical: Iris brown. No ptosis, icterus, or injection over sclera. Unable to fully visualize eyes for EOMI due to mental status. Fundoscopic exam: deferred. Visual acuity deferred.
Ears: Symmetrical: No TTP over tragus, lobe or helix. AU-EAC cerumen noted. TMs pearly gray, no injection or bulging TM noted. Whisper test deferred. Weber/Rinne deferred.
Nose: Septum midline. Patent airway. No rhinorrhea noted. Inferior turbinates observed. No hematoma, discharge or foreign body.
Mouth/Throat: Teeth intact and no evidence of loose teeth or dentures. No sweetness on breath or halitosis. Tonsils present grade 2. Uvula midline.
Lungs: Tachypneic rate. Clear to auscultation. No adventitious lung sounds.
Heart: Tachycardia. Regular rhythm without gallops, skips or murmurs.
Abdomen: No general or rebound tenderness. No palpable organomegaly.
Gentitourinary: Pubic hair evenly dispersed. Tanner stage5. Circumcised penis. No discharge noted. Edemotous scrotum over both testes. Malodorous with noted lesions over scrotum anteriorly.
Neurological: Alert, but unable to answer in complete sentences.
Musculoskeletal: deferred.
Differential diagnosis:
- DKA
- Septic shock
- AKI
- Fournier’s gangrene
- Necrotizing fasciitis
- Testicular torsion
- Rhabdomyolysis
CXR- obtained. Unremarkable (wet read)
Head CT: No intracranial hemorrhage, territorial infarction or mass lesion
Pelvis CT: extensive subcutaneous emphysema seen in the anterolateral abdominal wall bilaterally more in the right extending into the perineum and scrotum. (findings= fasciitis)
Orogastric tube placed.
A/P) 26 y/o male in acute distress with altered mental status, suspected ketoacidosis, septic shock with scrotal edema. Started 2 large bore IVs. Blood cultures obtained and empiric antibiotics. Intubated (7.0mm ET) due to respiratory rate and chance of aspiration. CXR-confirmed ET tube placement.
Pt admitted to ICU 9-100 block for continued sepsis workup.
Obesity
Uncontrolled HTNà labetalol 20mg IV titrate q4 hours
Diabetes mellitusàNovolog 10U IV q8 hours. Monitor sliding scale
Infectious disease consult
Pulmonologist consult
Surgical consult
Urology consult
Interventional radiologist consulted for central line access.
Update:
Patient is not compliant with diabetic medication and blood pressure regimen. Admits to unhealthy diet.
Central line placed left internal jugular via ultrasound. Confirmed with CXR.
Surgical debridement performed of scrotum, penis, perineum, right/left inguinal regions and right abdomen. Consent obtained by other and counseled about chances of infection, losing both testicles and penis.
Clindamycin, vancomycin, linezolid & meropenem.
Nephrology consult
Repeat surgical wound debridement in OR w/ plastic surgeon. Excised more necrotic tissue spreading to right lower abdomen. Pt extubated day#13.
Hemodialysis catheter placed in right internal jugular. Cr: 6.6 BUN 92 K 6.6
Patient has received repeat wound debridement over the past several weeks. 17Jan skin graft taken from upper/inner thigh and planted over right lower abdomen, penis, testicles, and perineum.
Patient is currently in ICU day 51.
_____________________________________________________
Article:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4452988/pdf/i0020-8868-100-5-934.pdf
Fournier’s Gangrene- A Summary of 10 Years of Clinical Experience(1)
I chose this article because it related most to my patient and his comorbidities. The article also describes a substantial sample size of patients with Fournier’s gangrene. Although the article is based in Turkey, the identification, diagnosis, treatment and prognosis is the same. Surgical debridement is of utmost importance in the initial stages of the disease. This article describes all of these important features and focuses on patients with diabetes mellitus. Based on the article nearly every patient had diabetes and the majority were infected with E. coli. With early identification prognosis was relatively good, however patients still needed intensive skin grafts and other surgeries to manage the groin infection.
____________________________________________________
Typhon:
____________________________________________________
Site Reflection:
During my first site reflection I presented a relatively “weak” H&P. The patient was seen by surgical team as a new patient for skin tags. For that initial visit I completed a full H&P on the patient and presented it as such. The following week I was in the operating room for a minor procedure which involved the removal of the skin tags. My site evaluator was looking for something a little more “interesting.” Nevertheless, he graded my H&P and gave me critical feedback for the next assignments. The following site visit was much more productive and interesting. The patient I presented during the second site evaluation was much more interesting and complex. The patient was diagnosed with Fournier’s gangrene and spent my entire rotation in the intensive care unit. The use of the medication drug cards is a great idea to keep up to date with the medications you see in the field as a student. My site evaluator gave my positive feedback and good suggestions on how to get the most out of my surgical rotation.
____________________________________________________
Rotation Summary:
My first rotation was on general surgery service at a 300 bed hospital in Brooklyn New York. I did not quite know what to expect for this rotation and I was approaching this experience with a little apprehension. The reason for these feelings was simply because of the lack of daily hospital function and understanding the flow of how things operate. Within the first few hours of being at the hospital I learned crucial medical skills to help better my proficiency and better the outcomes of my patients. A leading example is the importance of knowing the patient’s vital signs you are rounding on. At any moment the attending or resident might ask what the latest vitals are and how they have been over night. Another important anecdote that I learned within the first day is the importance of asking the patient, “Any changes overnight?” This question gives the surgical team a quick answer on post-operative complications. Follow up questions that the surgeons stressed were eating and drinking capabilities, change bowel habits, and if/frequency of urination.
The general surgery mentality for an inpatient service is to provide a surgical perspective for patients. The best way to describe this would involve a patient with a small bowel obstruction who is not seeing relief with contemporary measures. A surgical consult is called from the medical staff and the patient is quickly assessed. However, if the patient has any comorbidities that inhibits their ability to have surgery it’s the medical teams issues to correct. An example would be elevated blood glucose prior to a surgical procedure. If a patient has a blood glucose level of 300mg/dl they will more than likely not be going to surgery, unless it is an emergency. An absolute contraindication to any surgery is a patient in diabetic ketoacidosis (1). There are other indications when surgery may not be warranted including systemic infection, low cardiac ejection fraction and severe kidney issues (injury, infection).
This rotation has allowed me to see patients in crisis and yet comfort patients with minimal complaints who just need a little reassurance. I had great experiences in the operating room seeing patients who needed life-saving surgery. These patients had conditions like Fournier’s gangrene, adenocarcinoma of the colon or breast cancer that needed resection. The post-operative care for these types of patients were extensive and thorough which lead to another important aspect of the surgical team. The necessity to provide adequate care after surgery involves a strong knowledge of the patient’s history and being able to follow the patient as thoroughly as possible. This was another important aspect I learned on this rotation. It is important to trend the patient’s lab work and medications. One of my patient’s white count went from 8,000 to 17,000 in 36 hours. This tied into my first question I noted earlier, about changes over night. I made sure that the attending knew of the changes that occurred during morning rounds and worked with him to start antibiotic therapy and start a sepsis workup.
This rotation has taught me so much and I cannot adequately put on paper. The hours were long and the days were stressful. The operating room is truly an organism in itself. The scrub techs, the scrub nurses, anesthesiologists and the surgeon themselves provide a well-rounded team and provide excellent healthcare to the people they service.
(1) Pestena, C. Dr. Pestena’s Surgery Notes, Third Edition. Chapter 3. 2017. Kaplan Publishing.


