Case Study
Mr. R is a 70-year-old man who comes to see you in clinic accompanied by his wife because she is concerned that his memory is getting worse. She states that for the last few months he has been getting lost driving 20 miles from his home to his local VA hospital, where he volunteers. He has done this job twice a week for 25 years.
Mr. R’s past medical history is notable for chronic leg pain resulting from an injury during the war in Vietnam. He also has gout. Mr. R is a retired accountant. He completed 4 years of college. His physical exam reveals an alert, pleasant man.
His medications are
●Paroxetine, 20 mg daily
●Methadone, 20 mg 3 times daily
●Meloxicam, 7.5 mg daily
●Acetaminophen with codeine (300/60), 2 tablets 3 times daily
●Allopurinol, 300 mg daily
On examination, his vital signs are normal. He answers about half the history questions himself but turns to his wife for assistance with details about doctors he has seen and the medications he takes. He and his wife deny any symptoms of depression, although they note this has been a problem in the past. He has taken paroxetine for years.
His physical exam is normal except for evidence of bilateral knee osteoarthritis. Except for his mental status, his initial neurologic exam, including motor, sensory, and reflex examination, is normal. Further history revealed that the patient’s wife had taken over bookkeeping because a few bills had gone unpaid during the last 3 months. The patient was given the Mini-Cog and scored a 2 out of 5. Consideration of the NINCDS-ADRDA criteria showed him to have dementia with deficits in 2 or more areas of cognition (orientation, visuospatial and executive functioning, attention and working memory, and memory). At the time of the visit, it was not clear whether his cognitive functioning was worsening, and there were no disturbances in consciousness. The plan was made for initial laboratory work to be done and for a 3-month follow-up visit. Given that he was taking multiple psychoactive medications, his regimen was scaled back to the minimum doses necessary to control his pain. Initial laboratory evaluation, including CBC, TSH, basic metabolic panel and LFTs, vitamin B12 level, and rapid plasma regain, was normal. He was able to wean his medications and felt like he had a little more energy. On a follow-up visit 3 months later, the patient’s wife reported that he was no longer driving to his job as it had become too difficult. On physical exam, his language skills had worsened, and he frequently answered questions with short affirmative phrases and nods that were often contradicted by his wife. (He would subsequently agree with her.) A CT scan with contrast was ordered and showed only cerebral atrophy.
S) 70-year-old male, with past medical history of chronic leg pain due to injury and gout, presents to the clinic with his wife due memory loss concerns. The wife explains that Mr. R’s memory has gotten worse, especially while driving to his job x 2 months. He has held job 2 x weekly for the past 24 years. Wife has also noticed bills going unpaid and has taken over bookkeeping for the household x 3 months. Patient answers questions, but not to the extent expected. The wife has to assist or contradicts the answers the husband provides. Patient and wife deny any symptoms of current depression, but admit to previous depression and paroxetine (20 mg daily). Denies depression…(ROS here, Didn’t mention in text)
PMH: osteoporosis bilat knee.
Depression: controlled with SSRI
Gout: controlled with Allopurinol
Meds:
Paroxetine 20mg daily: depression
Methadone 20 mg 3 times daily: pain management knees
Meloxicam 7.5 mg daily: pain management knees
Acetaminophen with codeine (300/60) 2 tablets 3 times daily: pain management knees
Allopurinol 300 mg daily: gout
ALL: ?? Text doesn’t say.
O) WNWD male NAD A&OxIII. Good posture. Good hygiene. Noted dysphasia upon questioning. Unable to complete full sentences & appears to be searching for words while questioning. Good eye contact.
Vital signs: unremarkable.
Neurological exam: non-ataxic gait.
CN II-XIII grossly intact.
Muscle strength 5/5.
DTRs intact.
Cerebellar function: rapid alternating movements intact. Heel strike & finger to nose adequate.
Romberg: Neg
*mini-Cog score: 2/5
* NINCDS-ADRDA criteria showed dementia with deficits in 2+ areas of cognition
Lower extremities: FROM in all fields non-load bearing. Noted TTP over patella & popliteal space. Apley’s, Drawers & Varus/valgus Neg.
Laboratory tests: CBC, TSH, BMP, LFT, Vit B12, & RPR. Unremarkable.
A) 1. Alzheimer’s Disease: Dementia- likely due to wife’s consistency with cognitive function at home. Confirm w/ head CT showed cerebral atrophy.
DDx: late stage syphilis- R/O w/ RPR
Cerebral tumor- R/O w/ head CT.
CVA- Unlikely due to adequate neuro exam.
2. Osteoarthritis- Continue Methadone, PO 20 mg iii qd. Tylenol #3 (300/60) PO, ii TID. Meloxicam, PO 7.5 mg i qd.
3. Gouty arthritis- Continue Allopurinol, PO 300 mg i qd. Recommend diet changes w/ food low in uric acid (red meats, etc.)
4. Depression: Continue paroxetine, PO 20mg i qd.
P) 1. Reassurance to pt & wife.
2. Rx regimen scaled back to lowest dose.
3. Refer to psychiatry for further evaluation & management of cognitive degeneration. Appointment made w/ front desk for 14NOV18 @ 0930 w/ Dr. Brugna.
4. RTC within 3 months or sooner if symptoms worsen.
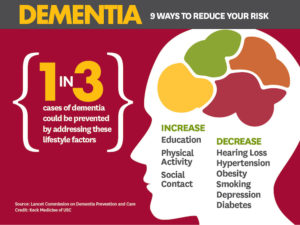
Summary: The medical conditions delirium and dementia are both related to neurological dysfunction, and a change in mental status. General examination findings are often vague and need to be differentiated between chronic and acute cognitive changes. These changes are crucial in acquiring an accurate diagnosis for the patient. Delirium is an acute condition, and is often reversible. Delirium presents typically with disturbances in both attention and awareness. These disturbances tend to fluctuate in severity over the course of the day. Thorough history taking and physical examination findings are necessary to see a direct cause of delirium which could include medical conditions and substance intoxication/withdrawal. In contrast, dementia is often chronic and almost always impossible to reverse. Dementia is classified as a major neurocognitive disorder, and features significant cognitive decline from a previous level of performance in 1 or more cognitive domains (i.e. learning and memory, language, social cognition, etc.) These deficits will interfere with the patient’s independence in activities of daily life (ADL). Due to the patient’s decline in cognitive status, loss of ability to perform higher-level tasks, and the patient’s advanced age, it is most likely that Alzheimer’s Disease (AD) is the diagnosis. This is the most common form of dementia and is often diagnosed as a process of elimination. In other words, different diseases are sought out and if unfound, diagnosis leads to AD. AD most commonly occurs after the age of 65, and features functional impairments in addition to memory loss. As the disease progresses, global cognitive impairment develops and the patient will be unable to independently accomplish even the most basic ADLs.
References:
Stern, S. C., Cifu, A. S., Altkorn, D. (2014). Symptoms to Diagnosis: An Evidence-Based Guide. Delirium and Dementia. 3rd Edition. New York. Electronic source.


